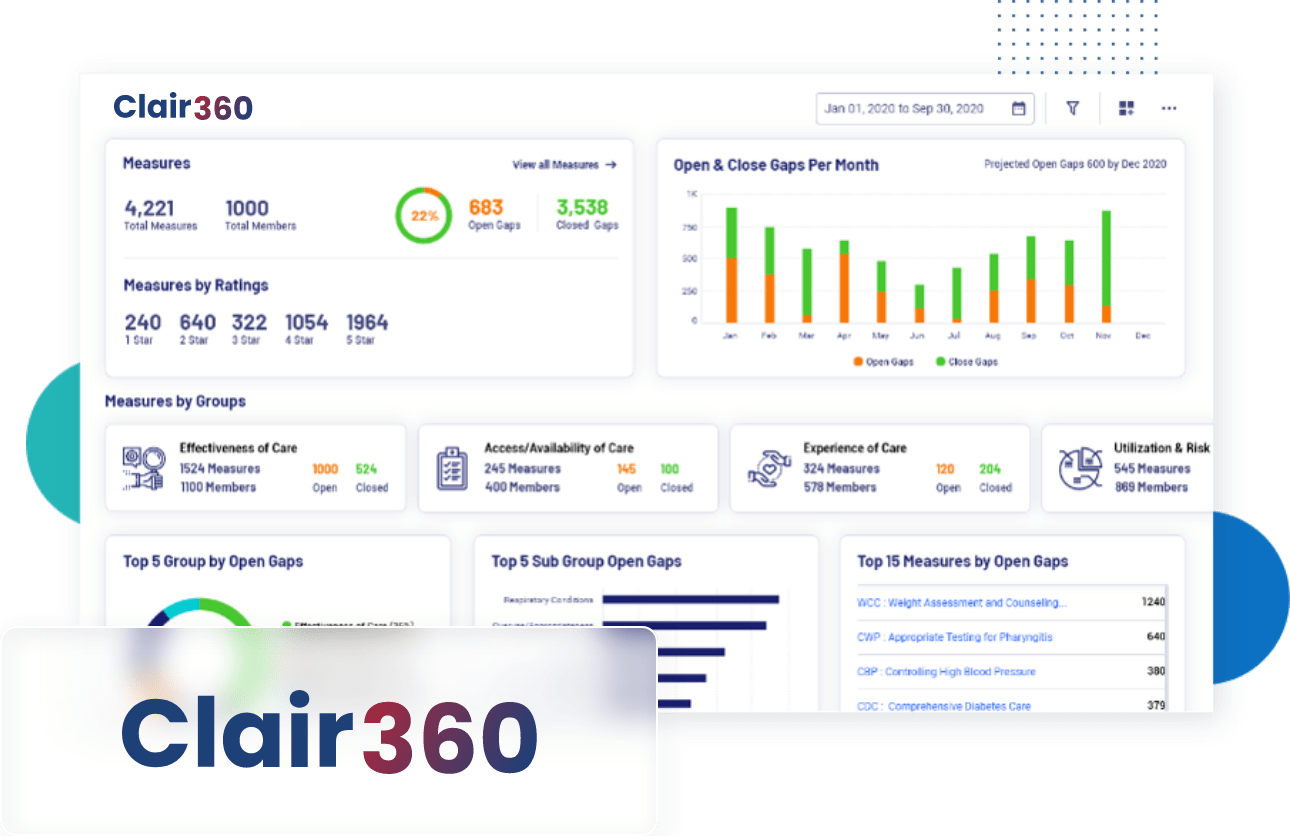
Clair360, a cutting-edge Snowflake Native App designed to transform the way payers and providers analyze patient data for HEDIS measures. Clair360, is an affordable tool to empower your quality program, which is also certified by NCQA for HEDIS measures. It offers a comprehensive suite of tools to streamline data analysis, facilitate data conversion, and ensure effortless submission to NCQA for star ratings.
Clair360 helps your organization to run scheduled quality analysis and ensure Data Security and Compliance. This provides you with insights such as
- Identification of Improvement Areas.
- Decision-making for enhancing care quality.
- Comprehensive analysis of quality data.